Haematological cancer, also known as blood cancer, is a type of cancer that starts growing either in blood-forming tissue, such as bone marrow, or in cells that are part of the immune system. For instance, leukaemia, lymphoma, or multiple myeloma are haematological cancers.
Specifically, multiple myeloma (MM) is a type of haematological cancer that is mainly known to trigger an uncontrolled expansion of plasma cells, which are responsible for producing the antibodies that protect us from disease [1]. If plasma cells expand more than they should, there is an excessive production of antibodies, particularly of one type of antibody: the M-protein. High levels of M-protein are associated with a series of symptoms such as high calcium levels (hypercalcaemia), anaemia, bone pain, fractures, recurrent infections, and kidney failure [2].
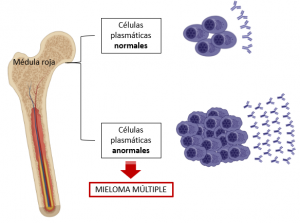
It is worth noting that MM is the second most common haematological cancer: it is accounted to be around 1% if compared with all types of cancers but, when it comes to blood cancers, its incidence rises up to 13%! [3]. In addition, its worldwide prevalence has increased by 126% since 1990, and it is most commonly found in the elderly, with 85% and 60% of diagnoses made in individuals over 55 and 65, respectively [1].
The cause of MM remains unknown, although some studies have found that age, sex, genetic background, and obesity may be considered possible risk factors. Environmental hazards such as exposure to solvents, herbicides, insecticides, and ionising radiation may also be the cause of triggering this this disease [3].
Did you know, however, that the immune system is essential to protect us from developing cancer? Yes, the immune system is responsible for the constant elimination of tumour cells, preventing them from spreading throughout our bodies and damaging our organs. Nevertheless, it has been observed that immune system cells do not function properly in patients with MM, and this causes malignant cells to multiply and migrate from the bone marrow to other regions of the body, and thus triggering severe symptoms in patients [1].
If the failure of the immune system leads to developing MM as well as causing serious side-effects in patients who suffer this disease, could we then use different strategies that strengthen or stimulate our immune system as a treatment? In short, the answer is yes, we can!

The strategies currently being studied to tackle MM through strengthening the immune system can be divided into two blocks. The first block refers to the use of drugs that target tumour cells. Some of these drugs include immunomodulatory drugs (IMIDs), which regulate the inflammatory environment in the bone marrow and also prevent the progression of MM by inhibiting the formation of new blood vessels, which are needed to transport nutrients and oxygen to tumour cells [4,5]. On the other hand, the second block includes those agents that are responsible for assisting anti-tumour cells: cells that directly attack tumour cells and cause their destruction (i.e., natural killer cells and cytotoxic T cells), cells that detect the presence of tumour cells and alert other specialised cells to cause their destruction (i.e., dendritic cells), and cells that activate and direct a wide variety of immune cells to act against the tumour (T-helper cells); among others. In this line, although we have become more and more familiar with using vaccines to deal with viral or bacterial infections throughout the past years (and even more during this pandemic), did you know that vaccines can also be used to induce specific anti-tumour activity? Essentially, this response is triggered by stimulating the anti-tumour cells mentioned above [4].
Thanks to treatments being improved year after year, the median survival of patients with MM now exceeds 7 years, although it is highly variable depending on the risk factors of the disease [1]. Despite dramatic therapeutic progress, however, MM remains an incurable disease as most patients end up developing multidrug resistance [6]. Consequently, the development of new treatments is crucial to reduce the high impact MM can have on this subset of patients. Hopefully, the advances in technology can soon lead to a better diagnosis and treatment for MM patients.
By Olaia Akesolo Atutxa, MSc student in Molecular and Cellular Biology.
More information: