Cancer and the increase in resistance to antimicrobial drugs are two of the greatest challenges for the world population. According to the World Health Organization, cancer kills more than 8 million people annually. Antimicrobial resistance is currently responsible for the death of about 1 million people. Moreover, it is estimated that the problem of antimicrobial resistance will worsen; by the year 2050, infectious diseases caused by bacteria resistant to antibiotics could be responsible for the death of 10 million people [1,2,3].
These forecasts make the search for alternative treatments, both for cancer and infectious diseases, increasingly necessary. This is where light can play a key role: the possibility of using light as a treatment may surprise, but there are multiple precedents throughout history.
The origin of the therapeutic use of light dates back, at least, to the early days of Hindu culture and the civilization of Ancient Egypt. The Atharva-Veda book and the Ebers papyrus, both documents over three thousand years old, describe the application of plant extracts to the skin before exposing it to sunlight to treat diseases such as psoriasis or vitiligo. In Ancient Greece, Hippocrates, known as the father of medical science, recommended sunlight for the restoration of health. Similarly, Persian scholar Avicenna wrote about the benefits of sunbathing in moderation. The Romans also used sunlight as a treatment, especially for skin diseases. Furthermore, it should be noted that, in Muslim Spain, the Andalusian scientist Ibn al-Baitar, in his book Kitab Al-jami li-mufradat al-adwiya wa al-aghdhiya (translated as “Compilation of medicines and food”), described the treatment of vitiligo with the application of a mixture of honey and powder of seeds of the Ammi majus plant, followed by exposure to sunlight [4,5].
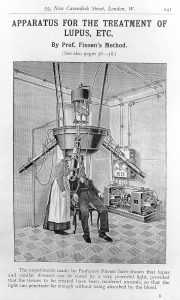
Figure 1. Sketch showing an innovative apparatus for the treatment of lupus. Source:Wikimedia.
With the fall of the Roman Empire and the spread of Christianity, the therapeutic use of light fell into oblivion until the beginning of the 19th century. Even so, it is considered that phototherapy – or light therapy – was not rediscovered until the beginning of the 20th century, when Oscar Raab, in Munich, published the first study on this topic. On the other hand, Dr. Niels Ryberg Finsen, Danish doctor and scientist, won the Nobel Prize in Medicine in 1903 for the use of light as therapy by publishing the first book on phototherapy and creating several lamps that he used to treat skin infections such as smallpox and lupus vulgaris, the latter being a form of cutaneous tuberculosis (see Figure 1). At the same time, the Germans Tappeiner (pharmacist) and Jesionek (dermatologist) conducted the first clinical studies in patients with tuberculous, syphilitic or skin cancer lesions. The lesions improved when they applied a compound called eosin and it was irradiated with light [4,6].
In the following decades, it was discovered that, if natural compounds called porphyrins were irradiated with light, these reacted with the oxygen in the environment, giving rise to reactive oxygen species (ROS). ROS are highly toxic and capable of destroying microorganisms or cancer cells, thus the operation (mechanism of action) of this treatment called photodynamic therapy was demonstrated. Currently, many compounds related to eosin or porphyrins are used, in addition to many others that are being investigated for their property of reacting with oxygen when they are stimulated with light. On the other hand, much progress has also been made and research continues on the use of different types of light and how to apply it. Overall, it makes the use of photodynamic therapy to treat infectious diseases and cancer a great alternative that is being used more and more [6,7].
The future of this therapy depends on continuing research. Thereby, we will be able to continue advancing in this line of a long history but with a lot of potential to develop, especially in the current context where both cancer and antimicrobial resistance are two of the greatest challenges in the clinic.
Specifically, in our studies, carried out mainly at the Miguel Servet University Hospital in Zaragoza and the Aragon Institute for Health Research (IIS Aragon), both in Spain, it is shown how some of the most pathologically relevant microorganisms, which are part of the main ones involved in the problem of antimicrobial resistance (that is, Staphylococcus aureus and Pseudomonas aeruginosa3), die after applying photodynamic therapy [8,9] (see Figure 2). In addition, we also investigated the use of very simple and cheap compounds such as methylene blue or rose bengal [10,11,12,13] as well as other more complex compounds [9]. These compounds are themselves harmless, and only when they are irradiated with adequate light, they trigger their toxic effect on microorganisms.

Figure 2: Bacterial culture plates. Left, without applying photodynamic therapy, center and right using different doses. Bacterial growth is completely avoided on the right. Image credits: ® Vanesa Pérez Laguna.
We have also worked to incorporate the compounds into common materials to make these materials self-disinfectant so that they are not a source of transmission of infections [9,14,15]. Finally, we have investigated the use of different lights, including sunlight, in order to reduce the use of complex irradiation devices and make photodynamic therapy much easier and cheaper to use [12,16].
* * *
By Vanesa Pérez Laguna, post-doctoral researcher at the Max Planck Research Group Evolutionary Cell Biology, Max Planck Institute for Evolutionary Biology (Germany).
More information:
- Bush K, et al. (2011).
- Post: Antimicrobial resistance. Source: World Health Organization (2020).
- Boucher HW, et al. (2009).
- Sellera FP SC and Hamblin MR (2017).
- Szeimies, et al. (2018).
- Hamblin M. (2008).
- Pérez-Laguna V, et al. (2018).
- Pérez-Laguna V, et al. (2020).
- Beltrán A, et al. (2016).
- Pérez-Laguna V, et al. (2017).
- Pérez-Laguna V, et al. (2018).
- Soria-Lozano, et al. (2015).
- Pérez-Laguna V, et al. (2017).
- Felip-León C, et al. (2017).
- del Valle CA, et al. (2020).
- Pérez-Laguna V, et al. (2017).